Understanding the UK’s public health workforce
by David Kidney, Chief Executive, UKPHR 
Introducing the UK’s public health workforce
When all is said and done, the public health profession in the UK is a small grouping within the health and social care workforce. Yet, for several reasons, it is really quite difficult to access accurate and comprehensive data about the demography of this vital group.
In my work at the Public Health Register, and in my membership of the advisory People in UK Public Health and the Standing Group on Local Public Health Teams in England, I am struck by the absence of a single, central source of up to date and usable data for public health workforce planning purposes.
In England, there is a long-running project to devise a minimum data set for the public health workforce, but any conclusions from this work still seem to be far off. Previously, the NHS Electronic Staff Record was used, but following the changes to public health organisation in England brought about by the passage of the Health and Social Care Act 2012, with basically the NHS employer replaced by multiple employers, there is no longer a single source for this data. At the same time, the divergence in practice and organisation in the four nations has made the challenge of collecting, assessing and publishing this data for workforce planning purposes more complex.
There is perhaps a broader point, too, about public health being a multi-professional, multidisciplinary endeavour, which is a great strength but inevitably brings a complexity of each profession having a different system.
Past work to develop fuller information includes:
- Multiple publications by the Centre for Workforce Intelligence (now archived) including a public health specialists stocktake, the extent of the core public health workforce in England, the extent of the core public health workforce in Scotland and a public health scientists stocktake;
- Health Education England reported on public health specialist capacity in England;
- The Royal Society for Public Health published reports on Understanding the UK’s wider public health workforce and Rethinking the public health workforce.
More recently, UKPHR contributed to a Public Health England (PHE) project run by Anna Sasiak and David Chappel to ascertain what other data was available. I have compiled the following information based on this work in particular.
I hope that, by publishing this information, I will stimulate further interest in developing the evidence base about the extent of the core public health workforce in the UK. This kind of evidence is what we need to consider when we embark on workforce planning and keeping the public health function fit for purpose going forward.
Recruitment to specialty training
Data from Health Education England (HEE) and the Faculty of Public Health (FPH) confirm there is no problem with recruitment to public health speciality training: there is 100% fill rate for all posts in the UK with 9 applicants per place. The average age of starting specialty training is 32 and of leaving training around 39.
UKPHR contributed to a project by David Chappel at PHE to determine the number of people joining specialist registers:
- General Medical Council (GMC);
- UK Public Health Register (UKPHR); and
- General Dental Council (GDC).
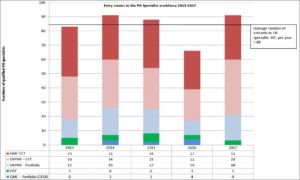
The project involved examining new entrants per year from different routes. It found that most new entrants joined the specialist public health workforce via the specialty training route as the following table shows:
As the table shows, the average number of entrants into the specialist workforce each year over a five-year period has been 84. In general, there are approximately 30 who complete training and join GMC’s register and 30 who complete training and join UKPHR’s register, with about 15 a year joining UKPHR’s register by a portfolio assessment route, smaller numbers joining GMC via the CESR route and another small number of GDC registrants.
An ageing workforce
Further data on career time lines for specialists comes from:
- FPH on recruitment as regards completion of training (‘CCTs’ issued) and Consultant advisory appointment committees (‘AACs’)
- HEE (on trainees)
- GMC, UKPHR and GDC as per the table above.
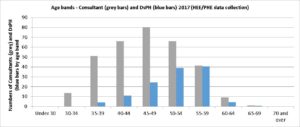
On average, Registrars spend 6 years in training and start to enter the PH specialist workforce from their early to mid-30s.
Directors of Public Health (DsPH) tend to get their first appointment in their 40’s or 50’s after around seven years in post as a public health specialist. The age pattern is as we might expect for a senior workforce:
Although the national picture for DsPH appointments is relatively stable, at local level this can and does play out differently. At any one time there will be some regions with a relatively stable DsPH workforce and others supporting recruitment for several interim and substantive DsPH vacancies.
It would be helpful to have enough evidence to enable system leaders and others to look at patterns to distinguish national trends from local issues, so that support can be targeted effectively.
Anecdotally, a concern was picked up that DsPH are currently being appointed very quickly after appointment to their first specialist post. The data shows that, while this is happening, it is a small number each year and the typical first appointment remains at 7-8 years after registration.
Leadership development
The 21st Century Leaders Programme for Consultants who are aspiring DsPH (the provider is University of Birmingham) is now well-established. It aims to improve the readiness of this group of potential leaders for DsPH appointment.
PHE is building an alumni network from among the participants in this Programme to connect system leaders and build the pipeline for DsPH.
The Association of Directors of Public Health (ADPH) has developed a national coaching and mentoring network for DsPH. The mentoring scheme has become well-established and is expanding its reach.
PHE has commissioned a scoping exercise exploring the development of system leadership in consultants and speciality registrars to develop the pipeline in to DsPH.
Practitioner workforce
Earlier work on data collection experienced great difficulty in identifying the boundaries of the practitioner component of the core public health workforce. This would be in part because the workforce is widely spread across all communities and all sectors of the economy. It would also be a factor that job titles and job descriptions are so diverse.
The practitioner workforce might be regarded as the engine room of the public health function, be it front-line delivery of services to individuals and communities, managers of workforces, commissioners of services and providers of science, research and analysis. Both academic public health and healthcare public health will also provide key settings for many public health practitioners.
Past attempts to research the extent of the practitioner workforce have taken into account those from backgrounds as diverse as environmental health, nursing and sexual health. There is no doubt in my mind that our current understanding of this workforce needs to be more thorough and all-encompassing. It would be helpful for future research projects to home in on this shortfall in our knowledge and understanding.
Data Collection
There is continued work by the Department of Health and Social Care, PHE and HEE to develop a minimum data set for collection of information about local authority public health staff.
In the interim, consideration is being given as to whether to repeat the 2017 survey of DPH and PH Specialist posts (or something similar) in 2019.
PHE will do more work on the data obtained from FPH and HEE to refine our knowledge of career patterns and provide a baseline for future monitoring.
Alignment of activities
The Standing Group on Local Public Health Teams (which includes key organisations such as PHE, HEE, ADPH, FPH, UKPHR and the Local Government Association), chaired by Chris Bull, has DsPH issues on every agenda.
PHE’s People Directorate is increasingly working with Centres and Regions.
The Supporting Place Programme (CP9) has just started mapping all current work on the DPH role. This will link the range of activities around the DPH role including a refresh of statutory guidance for appointments and new guidance on opportunities in Integrated Care Systems.
People in UK Public Health provides advice on workforce issues to all four nation’s Health Departments.
Suggestions welcome
It would be great to hear from others who may have knowledge to share, expertise to offer or ides for taking forward our understanding of the public health workforce.
If you want to make suggestions, please get in touch with me at d.kidney@ukphr.org. I will be happy to respond to queries and to route your suggestions to the appropriate places in the public health system where your ideas may be taken up.



Comments are closed.